The Hidden Costs of ‘Free’ Preventive Care: When Medical Coding Meets Patient Reality
Exhibit A | Colon Cancer Screening
As a clinician and executive who has spent decades navigating the complexities of healthcare delivery, I never expected to find myself on the other side of a billing error that exemplifies so many things wrong with our current system. Yet there I sat, staring at a $1,500 bill for what should have been a fully covered preventive colonoscopy under the Affordable Care Act (ACA).
Now, two years later and many nights wondering about what if others have gone through similar issues, it is past time to give back and it seems the timing couldn’t be more critical. A landmark study published in The Lancet Oncology in January 2024 revealed a troubling global surge in colorectal cancer, with cases expected to increase by 31.5% by 2030. This rise is particularly pronounced among younger adults, with a stark 90% increase in colorectal cancer diagnoses among people under 50 years old from 1990 to 2019…alarming to say the least.
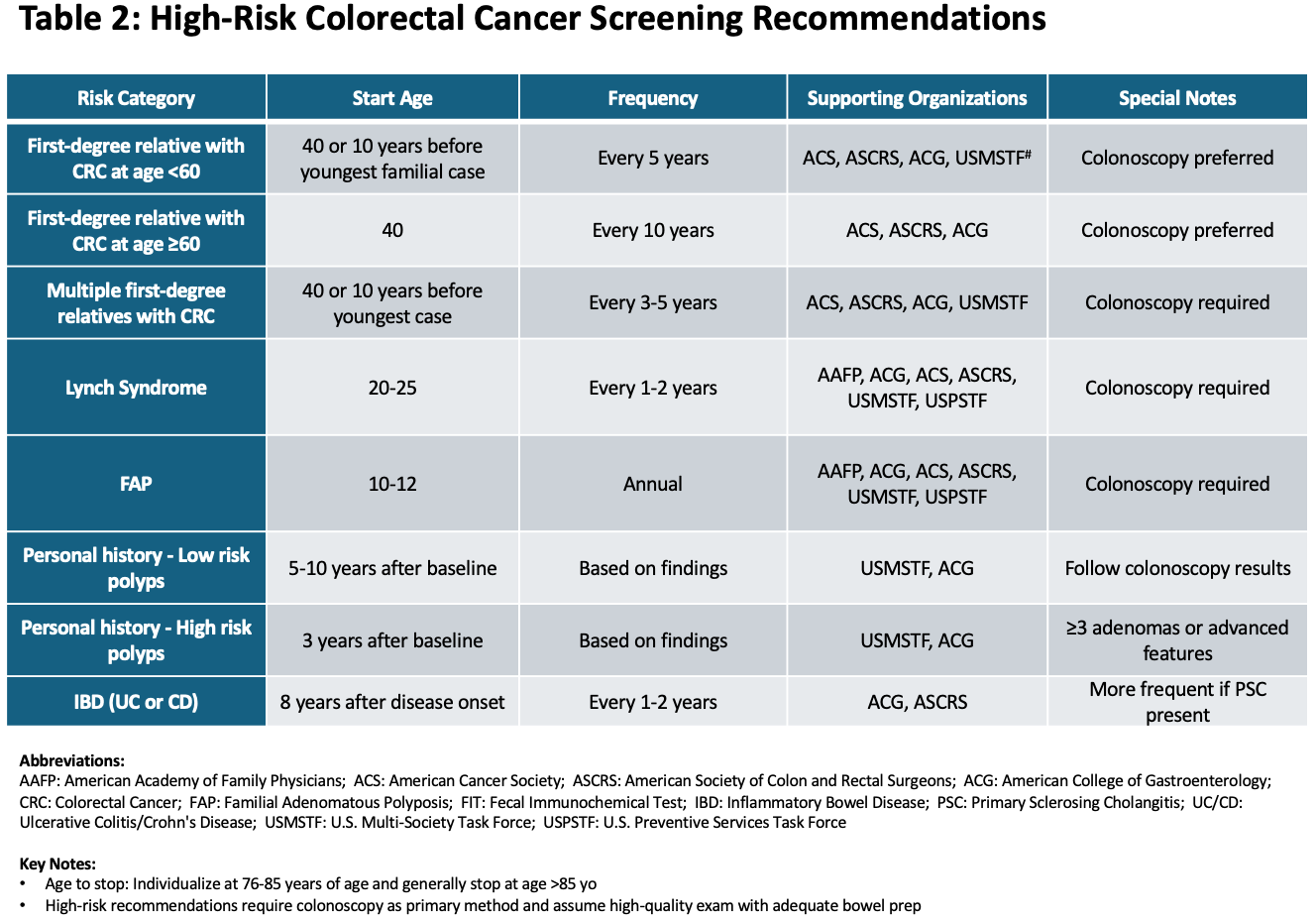
This shifting epidemiology has already prompted major changes in screening guidelines. The U.S. Preventive Services Task Force (USPSTF), whose recommendations directly inform ACA coverage requirements, lowered its recommended screening age from 50 to 45 years in 2021. While not completely reflected in USPSTF Statements, some other guideline recommendations provide specific recommendations for high-risk individuals which may include screening colonoscopy starting at age 40 years or ten years younger than the earliest diagnosis in their family, whichever comes first, and repeated every 5 years. These evidence-based guidelines (see Tables 1 and 2 below) form the foundation of preventive care coverage under the ACA, making it even more crucial that billing practices align with our expanding understanding of who needs screening and when.
Colorectal Cancer Screening Guidelines Summary
Like many patients, I had followed my doctor’s recommendation for early screening . At 44, I underwent a screening colonoscopy due to my family’s history of colorectal cancer — my father had multiple polyps removed before age 50, and my paternal grandmother died from the disease. During what should have been a routine screening, the gastroenterologist found and removed two precancerous polyps. As someone who understands provider clinical operations, revenue cycle management, payer services and healthcare policy, I thought I knew what to expect. Instead, I found myself caught in a maze of coding complexities and misaligned incentives that routinely undermine the ACA’s promise of free preventive care.
From Personal Challenge to Systemic Insight
My case perfectly illustrates both the problem and a path to resolution. After undergoing the colonoscopy at Allegheny Health Network, I received a $1,500 bill when my insurance, Blue Shield of California, processed the procedure as diagnostic rather than preventive pursuant to how the claim was submitted by my provider. Despite meeting all the criteria for preventive screening — including my age (44), first degree relative with polyps before 50 and family history of colorectal cancer — the removal of two precancerous polyps had seemingly triggered a reclassification of the entire procedure.
What followed was a journey through the labyrinth of healthcare billing that tested even my extensive background in payer operations, provider systems, and healthcare policy. After multiple exchanges with both Allegheny Health Network and Blue Shield of California, it initially seemed I was at an impasse.
When Allegheny Health Network’s billing team member cited WebMD as her source for clinical and coding guidance, I knew more authoritative sources were needed. I responded by directing them to the American Gastroenterological Association’s official Colorectal Cancer Screening coding guide, specifying exactly how my procedure should have been coded: CPT code 45384 or 45385 with Modifier 33 to indicate a preventive service, diagnosis codes Z12.11 and Z12.12 for the colorectal screening, codes Z80.0 and Z83.71 to reflect family history of polyps and neoplasm, along with any additional diagnosis codes potentially applicable based on pathology findings (e.g., D12.0, D12.4, and D12.8).
Crucially, I also cited official guidance from the U.S. Department of Health and Human Services (HHS) Affordable Care Act Implementation FAQs, specifically Question 5, which explicitly states that,
“The plan or issuer may not impose cost-sharing with respect to a polyp removal during a colonoscopy performed as a screening procedure.”
This combination of technical coding knowledge and policy understanding ultimately proved decisive. Through persistent advocacy and clear communication about the ACA’s preventive care requirements, Blue Shield of California attempted to work to remedy the claim submission errors with my provider and eventually agreed to cover the claim in full.
This resolution, while positive, raises a troubling question: what happens to patients without insider knowledge of the healthcare system? A January 2024 NPR investigation by Samantha Liss and Zach Dyer revealed this isn’t an isolated incident, documenting cases where patients face unexpected charges, from $600 surgical tray fees to full procedure costs, for supposedly “free” preventive care.
The Technical Reality Behind Billing Failures
Having led healthcare transformation initiatives, I’ve seen firsthand how well-intentioned policies can falter in implementation. The current coding and billing infrastructure wasn’t designed for the nuanced requirements of modern preventive care. When my gastroenterologist found and removed two precancerous polyps during my screening, it triggered a cascade of coding decisions that reflect this fundamental misalignment.
The complexity begins with the guidelines themselves. As shown previously in Tables 1 and 2, the USPSTF recommends several screening strategies, each requiring different coding approaches which drives the payor policy . The American Cancer Society adds to this complexity by recognizing that some patients may need earlier screening based on additional risk factors, not to mention evidence-based guidelines and statements from other professional organizations.
Unfortunately this is where the system lags in getting evidence into practice — 1) Getting adoption from clinicians, 2) aligning payer medical and benefits policies and 3) ensuring providers, operations, clinical documentation and billing processes are aligned and sophisticated enough to handle this variety while maintaining the preventive nature of these services. Medical coding exists at the intersection of clinical documentation, billing practices, and insurance policies. The NPR investigation revealed how facilities have begun unbundling basic supplies from procedure costs, creating new revenue streams that bypass ACA protections.
The NPR story highlighted Elizabeth Mellon, a Michigan teacher who was billed $600 for a surgical tray, captured the absurdity perfectly when she told NPR: “I thought preventive procedures were supposed to be covered at 100%.”
The problem extends beyond simple medical coding errors. Our current system struggles to handle procedures that begin as preventive but evolve into therapeutic interventions. This reflects a broader challenge: our billing infrastructure hasn’t kept pace with our understanding of preventive medicine and value-based care and even much less so with the broader billing and financial capabilities seen in other industries.
Innovation Opportunities: Reimagining Healthcare Billing
As someone deeply involved in healthcare innovation, I see these challenges as opportunities for transformative change. We need solutions that address both immediate pain points and underlying systemic issues that could be broken into the following elements.
Digital Infrastructure Modernization
Modern healthcare requires billing systems that can handle nuanced clinical scenarios. We need intelligent systems that can maintain the preventive classification of a procedure while accurately documenting therapeutic interventions. This isn’t just about better coding — it’s about creating digital infrastructure that aligns with our clinical and policy goals and supports the clinicians.
It seems we a critical need: our systems must be built on authoritative sources maintained against evolving evidence and official guidance, not general healthcare websites. Perhaps when billing teams can easily access and apply official guidelines from organizations like the American Gastroenterological Association and HHS, we reduce errors and streamline the billing to avoid surprises.
Value-Based Billing Alignment
The surgical tray billing issue highlighted by NPR demonstrates how fee-for-service thinking undermines preventive care. We need payment models that bundle appropriate supplies and services into preventive procedures, eliminating the incentive to unbundle charges. Some forward-thinking health systems are already moving in this direction, proving it’s possible to align financial sustainability with patient-centered care.
Automated Compliance and Verification
Healthcare organizations need better tools to verify preventive service coverage and catch potential billing errors before they reach patients. Machine learning and natural language processing could help identify coding patterns that frequently lead to inappropriate bills, enabling proactive corrections.
Transforming Promise into Practice
In all, this has strengthened my conviction that we must do better. The ACA’s promise of free preventive care represents a crucial step toward a more proactive, equitable healthcare system. However, delivering on that promise requires us to reimagine our approach to healthcare operations and billing. To shift from hindsight to foresight, I am left with some thoughts but more so questions:
Is there a path for patient to input risk factors that can be converted and reduced to appropriate codes (e.g., z-codes)? (Z-codes in general have poor industry adoption)
Which provider is the one who documents the information that is commonly missed, the ordering provider or performing provider? (this should inform educational support focus)
How many screening colonoscopies are done each year that manifest in these “surprise” bills that ultimately put patients into financial hardship?
How can we leverage digital health platforms to automate the capture and translation of patient risk factors into appropriate coding, reducing the current manual documentation burden?
What role should EHR vendors play in creating standardized workflows that ensure proper documentation of preventive intent across both ordering and performing providers?
Can claims data indicate any perspective to the scope and financial burden of this potential billing error?
In the meantime, it seemed relevant to share a process that may assist in avoiding such errors by leveraging best practices. Although only a simple resource, perhaps it may provide a foundation to prevent the kinds of errors that lead to unfortunate surprises. This isn’t just about following rules — it’s about honoring our commitment to preventive care and maintaining patient confidence in the healthcare system.
A Path Forward: From Insight to Action
My case resolution with Blue Shield of California demonstrates that proper coverage is possible when all parties understand and correctly apply existing guidelines. However, we shouldn’t require patients to have insider knowledge or wage prolonged appeals to receive their rightful coverage. The response to NPR’s investigation offers additional hope — Spectrum Health in Michigan stopped charging separately for surgical trays after being contacted by reporters. But we shouldn’t rely on journalism or individual advocacy to drive change.
The stakes are too high for incremental solutions. The article from Lancet Oncology had projections of a 31.5% increase in colorectal cancer cases by 2030 demands urgent action. We’re facing a future where colorectal cancer increasingly affects younger populations, with cases rising most rapidly among those under 50. This shift in disease demographics makes it even more critical that we remove barriers to early screening. As healthcare leaders, we must:
Invest in digital infrastructure that supports proper preventive care billing
Design workflows that preserve preventive classification while accurately documenting care
Implement automated systems to support simplification of billing so as to prevent errors
Evolve the transparency tools that help patients understand their medical and benefits coverage
Advocate for policy changes that create more timely improved paths for integrating evidence in policy while working to simplify preventive care billing
We need fundamental transformation toward simplicity in structuring, delivering, and billing payers for preventive care. This includes embracing digital innovation, aligning incentives across the healthcare ecosystem, and creating systems that work for both providers and patients.
As healthcare leaders, we have the tools and knowledge to solve these challenges, but the devil is in the details. With colorectal cancer cases rising dramatically worldwide and increasingly affecting younger populations, removing barriers is about saving lives. Our patients are counting on us to get this right.
Disclaimer: The views expressed in this article are my own and do not represent the opinions of my employer or any organization with which I am affiliated. While I have extensive experience in healthcare transformation and strategy, I am not a certified medical coding professional. The coding guidance provided is based on publicly available resources and should be verified with official coding authorities and guidelines. Readers should consult with certified coding professionals and their respective healthcare organizations for specific coding advice.
This article is based on personal experience as both a patient and clinician, extensive research, and discussions with healthcare policy experts and providers. It builds upon reporting by Samantha Liss and Zach Dyer for NPR/KFF Health News (January 2024), research published in The Lancet Oncology (January 2024), and guidelines from the U.S. Preventive Services Task Force and American Cancer Society.
For more information about preventive care coverage under the ACA, visit https://www.healthcare.gov/coverage/preventive-care-benefits/ and for Medicare, visit https://www.medicare.gov/coverage/preventive-screening-services.
Key References:
US Preventive Services Task Force, Davidson KW, Barry MJ, et al. Screening for Colorectal Cancer: US Preventive Services Task Force Recommendation Statement. JAMA. 2021;325(19):1965–1977. doi:10.1001/jama.2021.6238
Wolf AMD, Fontham ETH, Church TR, et al. Colorectal cancer screening for average-risk adults: 2018 guideline update from the American Cancer Society. CA Cancer J Clin. 2018;68(4):250–281. doi:10.3322/caac.21457
Shaukat A, Kahi CJ, Burke CA, et al. ACG Clinical Guidelines: Colorectal Cancer Screening 2021. Am J Gastroenterol. 2021;116(3):458–479. doi:10.14309/ajg.0000000000001122
Rex DK, Boland CR, Dominitz JA, et al. Colorectal Cancer Screening: Recommendations for Physicians and Patients from the U.S. Multi-Society Task Force on Colorectal Cancer. Am J Gastroenterol. 2017;112(7):1016–1030. doi:10.1038/ajg.2017.174
Sharma KP, Guo J, Arnold M, et al. Global trends in incidence and mortality of colorectal cancer by age and country income level, 1990–2019: A population-based study. Lancet Oncol. 2024 Jan:S1470–2045(24)00600–4. doi:10.1016/S1470–2045(24)00600–4
Liss S, Dyer Z. The colonoscopies were free. But the surgical trays came with $600 price tags. NPR; 2024 Jan 25. Available from: https://www.npr.org/sections/health-shots/2024/01/25/1226552799/
American Academy of Family Physicians. Clinical preventive service recommendation: colorectal cancer screening. AAFP; 2018. Available from: https://www.aafp.org/pubs/afp/issues/2018/0115/p111.html
American Society of Colon and Rectal Surgeons. Clinical practice guidelines: colorectal cancer screening and surveillance. ASCRS; 2023. Available from: https://fascrs.org/healthcare-providers/education/clinical-practice-guidelines
American Gastroenterological Association. Coding guide: free colorectal cancer screening . AGA; 2023 . Available from: https://gastro.org/practice-resources/reimbursement/coding/coding-guide-free-crc-screening